 Necrotizing soft-tissue infections (NSTIs), including necrotizing fasciitis, are rare but life-threatening conditions that require urgent medical attention. Prompt diagnosis and immediate treatment are critical to preventing severe complications, including limb loss or death. Understanding the signs, causes, and risk factors of necrotizing fasciitis can help individuals seek care quickly, which is essential for effective management and recovery.
Necrotizing soft-tissue infections (NSTIs), including necrotizing fasciitis, are rare but life-threatening conditions that require urgent medical attention. Prompt diagnosis and immediate treatment are critical to preventing severe complications, including limb loss or death. Understanding the signs, causes, and risk factors of necrotizing fasciitis can help individuals seek care quickly, which is essential for effective management and recovery.
What is Necrotizing Fasciitis?
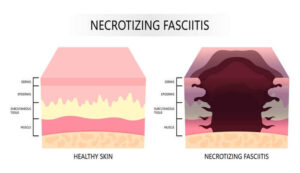
Necrotizing fasciitis is a rapidly spreading bacterial infection that attacks the skin, fat, and tissue covering the muscles (fascia). Often referred to as a “flesh-eating” disease, this condition can destroy tissue and muscle at an alarming rate, making early intervention vital. Although rare, necrotizing fasciitis can develop after minor cuts, scrapes, or even surgical wounds.
What are the Symptoms of Necrotizing Fasciitis?
Symptoms can escalate quickly, often within hours. Early signs include:
- Severe pain disproportionate to the wound or injury
- Redness, swelling, and tenderness around the affected area
- Fever, chills, and fatigue
- Skin discoloration or blistering
- Rapid spread of swelling and redness
As the condition progresses, affected areas may become dark or black due to tissue death (necrosis). Immediate medical intervention is crucial if these symptoms appear.
What Causes Necrotizing Fasciitis?
Necrotizing fasciitis is most commonly caused by group A Streptococcus (GAS) bacteria, although other bacteria such as Staphylococcus aureus or Clostridium can also be responsible. These bacteria can enter the body through:
- Cuts or scrapes
- Surgical wounds
- Burns or insect bites
- Blunt trauma that causes skin breaks
Risk Factors for Necrotizing Fasciitis
While anyone can develop necrotizing fasciitis, certain individuals are at greater risk, including those with:
- Diabetes or weakened immune systems
- Chronic kidney or liver disease
- Cancer or chemotherapy treatment
- Recent surgical procedures or wounds
- Intravenous drug use
How is Necrotizing Fasciitis Diagnosed?
Diagnosing necrotizing fasciitis often involves a combination of:
- Physical Examination: Assessment of pain, swelling, and tissue appearance.
- Imaging Tests: MRI or CT scans to identify tissue damage.
- Laboratory Tests: Blood work to detect signs of infection and inflammation.
- Tissue Biopsy: A sample from the affected area may be taken to confirm the diagnosis.
How Can I Prevent Necrotizing Fasciitis?
While prevention isn’t always possible, you can reduce your risk by:
- Practicing good hygiene and wound care
- Cleaning and covering cuts and wounds properly
- Seeking medical attention for any signs of infection
- Managing underlying health conditions like diabetes
DFW Wound Care Center specializes in the emergent treatment of necrotizing soft-tissue infections and other complex wounds. Our expert team utilizes advanced wound care techniques, including hyperbaric oxygen therapy, surgical debridement, and infection management.
We have immediate openings and are accepting new patients at our four clinics in Plano, Lewisville, Irving, and DeSoto. Don’t delay – contact DFW Wound Care Center today to receive expert care and prevent further complications.
Contact us
Schedule an appointment
with our specialists by contacting us or calling our:
